Cost Weight in DRG Costing is Driving Value-Based Healthcare in Saudi Arabia
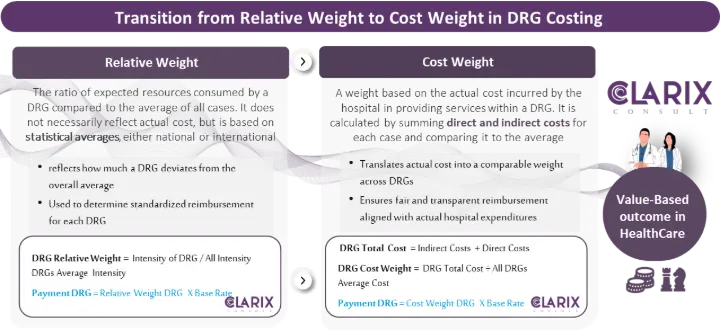
Two important concepts in DRG costing are Relative Weight and Cost Weight. While often used interchangeably, they serve different purposes and have distinct implications for how hospitals and insurers manage payments.
What is Relative Weight?
Relative Weight represents the complexity and resource intensity of a specific DRG compared to the average case.
It is a numerical index assigned to each DRG.
A higher relative weight indicates a case that is more resource-intensive (e.g., complex surgery with complications).
It is primarily used to normalize payments by showing how one case compares to another.
What is Cost Weight?
Cost Weight translates the relative weight into actual financial value, by linking it to a base rate (the national or agreed cost per weight unit).
The base rate is often determined by health authorities or insurers, considering average treatment costs and budget constraints.
Cost Weight is therefore the financial expression of relative weight, allowing hospitals to be reimbursed fairly for the resources used.
Why it Matters for Value-Based Healthcare
In traditional fee-for-service models, hospitals are paid for each service provided, which can encourage over-utilization. DRG costing, when linked with value-based principles, shifts focus toward outcomes and efficiency.
DRG costing, when linked to value-based principles, shifts the focus toward outcomes, efficiency, and fairness in reimbursement.
Key Benefits in the Saudi Context:
Fair & Transparent Payments
Insurers and hospitals operate on a standardized framework, minimizing disputes and aligning incentives.
Efficiency and Cost Control
Providers are encouraged to manage resources more effectively without compromising patient outcomes.
Supports Vision 2030 Transformation Goals
Aligns with the Council of Health Insurance (CHI) and Ministry of Health efforts to implement value-based reimbursement models.
Benchmarking Across Hospitals
Relative weights allow hospitals to be compared on performance and efficiency, while cost weights ensure that payments reflect actual costs.
Better Negotiations Between Insurers & Hospitals
Using DRG-based costing, pricing discussions are grounded in data and evidence, not arbitrary tariffs.
The Road Ahead
Saudi Arabia has already begun adopting AR-DRG standards, alongside the ICD-10-AM coding system, as part of its financing reform. Moving from relative weight (intensity-based costing) to cost weight (actual expenditure-based costing) is a critical step to ensuring a transparent, sustainable, and value-driven healthcare ecosystem.
Hospitals must strengthen cost-accounting systems to measure and report real costs.
Insurers must embrace cost weight–based payments to balance affordability with sustainability.
Regulators (CHI, MoH, Vision Realization Offices) need to define and update base rates to reflect actual cost structures and encourage high-quality, efficient care.
At ClarixConsult, we partner with healthcare providers, payers, and regulators to design, implement, and optimize value-based care and payment models, ensuring alignment with both local and international best practices